
Osteochondrosis of the lumbar spine is a dangerous disease of the spine that characterizes people 35 years of age and older. The natural wear and tear of the joints leads to the development of the pathology. In most cases, failure to see a rheumatologist in time can lead to disability. Modern medicine offers many effective treatments at the primary stage. Early diagnosis is the key to living a healthy life without limitations.
Lumbar Osteochondrosis - General Definition
Osteochondrosis of the lumbar spine is a dystrophic degenerative process of the formation of the cartilage of the intervertebral discs - the intervertebral discs.
Intervertebral discs provide the main functions of the spine - the ability to move and bend, and resist pressure. Due to the pathology, vital elements become thinner, deformed, vertebrae are aligned, and nerve endings and blood vessels are squeezed. Negative processes are accompanied by varying intensities of pain perception and limitation of motor function.
Pathology can cause changes in the connecting elements of the spine - cartilage, bone, discs and joints. It is caused by natural wear process and acquired joint disease or improper lifestyle.

reason
Osteochondrosis of the lumbar spine can occur for many reasons:
- natural or premature wear of the body;
- Excessive load on the lower back - lifting weights, working "on both feet" or a sedentary, "sedentary" lifestyle;
- Genetic susceptibility to joint diseases, such as rheumatoid arthritis;
- Violation of metabolism, leading to accumulation of toxic substances in the connection plate;
- Chronic diseases of the circulatory system. Nutrients and trace elements stop the proper amount of entry into cartilage tissue. Hypoxia can lead to the destruction of the intervertebral joints;
- Autoimmune Pathology.
Secondary factors may also trigger the development of lumbar osteochondrosis:
- chronic injuries, back bruises;
- More than 15-20% more than the weight standard;
- heavy or strength exercise;
- Often wear uncomfortable shoes. High heels, tights, rubber shoes or sneakers are the number one enemy of the spine;
- Changes in foot eversion;
- Scoliosis, kyphosis, diabetes, spinal tuberculosis;
- effect of low temperature.
clinical picture
The symptoms of lumbar osteochondrosis depend entirely on the nerve roots affected by the disease. The degree of compression of the vertebrae, the stage of the disease, and damage to the discs determine these signs.
Rheumatologists distinguish the following major symptoms:
- Violation of tactile sensitivity in the lumbar region. The numbness extends to the inner thighs and groin. May affect one or both limbs;
- There is a severe, severe pain in the lower back. Complete loss of mobility in the big toe, and characteristic numbness is observed;
- Loss of normal function in the foot and loss of sensitivity in the fingers, calves and outer thighs. In these parts of the leg, there are tonal and regular twitching episodes. On examination, there is no Achilles tendon reflex;
- If the disease affects the inferior nerve root artery, the muscles of the buttocks, back of the thigh, and perineum can be completely paralyzed. Motor function is severely impaired to the point of complete immobility.
Lumbar osteochondrosis affects not only the nerve endings of the spine, but also the blood vessels.
The following specific signs depend on the type of lesion:
- Changes in the patient's gait were observed when only the nerve roots were disturbed. The pain is not limited to the lower back area, but is present in all parts of the legs. Radicular syndrome is characterized by persistent pain. Usually only on one side. In the lower back, tingling and pain are noted. A little exercise can ease the pain.
- Compression of the blood vessels leads to perfusion in the buttock area. As a result, intervertebral disc hypoxia occurs. Pain in the buttocks, thighs, and lower back when walking. Remove completely after a night of rest.
Simultaneously disrupting the function of blood vessels and nerve roots can lead to irreversible deformation of the intervertebral disc. Spiny bone growths form in the movable joints of the lower back. This can cause severe pain and make normal natural movements impossible. Violation of posture, gait. As it progresses, complete paralysis may occur.
stage of disease
Osteochondrosis of the lumbar spine develops gradually and in several stages. Each stage has its own characteristics that determine the degree of progress.
- I'm on stage.The disc begins to slowly break down. This process can last from a few months to 2-5 years. It presents as mild pain, discomfort in the groin and femoral muscles. Noticed when walking or when the weather changes.
- Stage two.Collagen fibers of the spinal annulus are pulled into the negative process. The space between individual vertebrae is shrinking rapidly. Friction occurs, leading to severe pain flare-ups. Irregular gait, posture, stooping. Osteochondrosis of the lumbar spine is most often diagnosed during the second stage of the course.
- The third phase.Intervertebral hernia occurs. If the patient is not compelled to seek medical help for the symptoms of the second stage, it will no longer be possible to ignore the excruciating pain of the third stage. Deformation of the spinal bones and joints in the lumbar region is already irreversible. It takes a lot of effort to walk. This is due to pain and the inability to relieve pain with traditional pain relievers.
- Phase IV.Partial or complete impairment of motor function. At this stage, patients are assigned to a disability group. threatened with complete paralysis. It is impossible to perform important activities without taking multiple medications.

Diagnostic measures
Diagnostic measures include several techniques and begin with collecting a complete disease history. During an initial consultation with a rheumatologist, the following data were clarified:
- Careful analysis of the patient's complaints - the location of the pain, where discomfort is still felt, which parts of the hip are heavier, twitching, etc. ;
- Duration, regularity, nature of pain;
- When the first, even mild symptoms appear. How much time has passed since the last attack, what caused the discomfort and what factors helped to resolve it;
- The patient's surrounding living environment. Occupation, job, family burden, exercise and other factors that increase physical activity (house, garden, hobbies related to weight transfer);
- Check the patient's past or present medical history.
After collecting the clinical pictures, the rheumatologist conducts an external examination directly. During the examination, the gait, the anatomical position of the legs, arms, and torso relative to the spine are analyzed. Check your skin for changes - hyperpigmentation, peeling, eczema, rash, etc. An assessment of motor function is given.
Performing simple exercises - leaning forward, backward, raising arms and legs, turning the head, rotational movements of the pelvis, the patient allows the doctor to determine the degree of spinal damage in the lumbar region.
The final measure of external examination is the measure to determine the extent of nerve root damage:
- Symptoms Laser.The patient lies supine with legs alternately raised and knees bent. If this results in lower back pain, the reading is considered positive.
- Symptoms Dejerine.Ask the patient to tighten the abdominal muscles as much as possible. The occurrence of spinal discomfort indicates the development of lumbar osteochondrosis.
- symptoms inside. A sharp forward and backward tilt of the head can cause pain in the lower back.
- Symptoms Wasserman. With the patient supine, move the leg to the side as far as possible. In the presence of pathology, unpleasant pain in the groin and front of the thigh.
To confirm or rule out the diagnosis, ask the patient to perform an instrumental diagnosis. MRI is considered the most effective method for identifying osteochondrosis of the lumbar spine. The study showed the distance between the vertebrae, the development of tumors and skeletal deformities. Mental disorders may be contraindicated.
Computed tomography gives a fairly realistic picture of the disease in one plane (horizontal or vertical).
X-rays are only used in the final stages, when irreversible changes in the bone tissue of the spine begin.

Comprehensive Treatment of Lumbar Osteochondrosis
The pathological cause has not been fully elucidated. Scientific research in the field of spinal and joint disorders has not yet identified a sufficiently effective method to fully restore the intervertebral disc. Modern treatments are only aimed at eliminating external signs of the disease. Full recovery is currently considered impossible.
traditional medicine
A rheumatologist will prescribe medication based on a patient's general condition. Clinical pictures provide the necessary information to develop treatment regimens from multiple groups of drugs.
- Anesthetic.Prescribe injections, ointments, or broad-spectrum medications.
- Anti-inflammatory drugs (NSAIDs).
- Vasodilator.Remove tension from the waist and leg muscles.
- chondroprotective agent.Aims to rule out negative progression of lumbar osteochondrosis.
physiotherapy
Physical therapy procedures are an integral part of inpatient or outpatient treatment for lumbar osteochondrosis.
Include the following activities:
- Painkillers electrophoresis;
- magnetic therapy;
- Spa;
- Paraffin application.
Medications and physical therapy in the complex relieve acute pain and inflammation. But they are not guaranteed to stop the progression of the pathology. Just a course of 2-3 times a year and a responsible attitude of the patient will help to avoid regression and maintain general condition in satisfactory form.
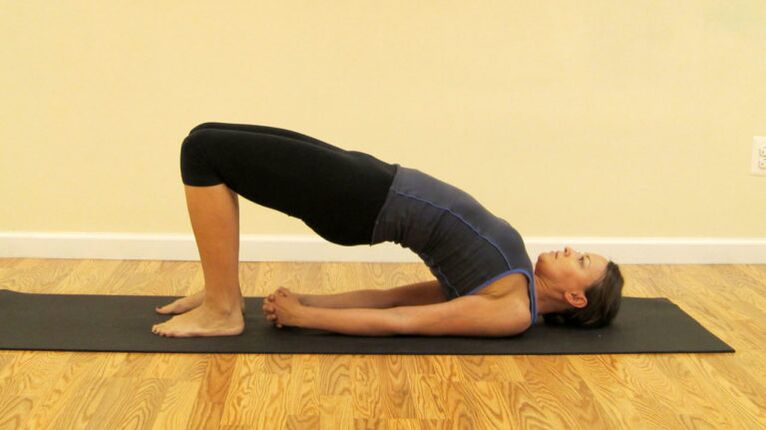
Sports Therapy and Therapeutic Massage
A set of therapeutic gymnastics exercises ensures that the blood circulation in the lower back is normalized and helps to eliminate the stagnant process. Only a physical therapist can prescribe exercises for clinical or home use. Typically, these are various gentle tilt and rotation movements in prone and seated positions. Not only does independent physical activity lead to no results, but it can lead to more disc displacement.
Manual therapy sessions help strengthen muscle tissue, allow blood flow to the affected lower back, and relieve tension. Experts begin by massaging healthy areas of the back to heat the muscles and improve blood circulation. It then reaches the affected area of the lumbar spine. The operating area includes the lower back, buttocks, thighs, calves and feet. Classes are held in regular sessions with a minimum of 10 sessions in 6 months.
Surgical treatment
It is indicated in the final stages of lumbar osteochondrosis to restore the motor function of the spine. Surgery remains the only option for patients with the following symptoms:
- Persistent pain syndrome that cannot be treated even with opioid-containing medications;
- Strong compression of nerve roots and significant displacement of the intervertebral disc;
- tumor, proliferation of bone tissue;
- Complete destruction of the vertebrae due to constant friction;
- paralysis.
Modern methods offer less traumatic methods of internal intervention. For example, endoscopy. The prognosis is good, with a short recovery period and few side effects.

replacement therapy
Lumbar osteochondrosis responds well to treatment with herbal and folk methods. Ointments, tinctures, and fee-based body washes are used to reduce swelling and pain. The most effective recipes include numbing and anti-inflammatory herbs:
- yarrow;
- aloe;
- Mint;
- St. John's wort;
- spruce or pine needles;
- wise.
The inclusion of these herbs in folk recipes is due to their medicinal properties and scientifically proven in traditional medicine. Treatment at home will help keep the lower back stable and prevent the disease from getting worse after complex treatments.
prevention
Although lumbar osteochondrosis is an incurable disease, its negative manifestations can be minimized. In the early stages, the disease is successfully treated and only requires prompt medical help. It is very important to fully adhere to the established treatment regimen and to follow the advice of the rheumatologist.



















